Strokes 101: Prevention, warning signs and risk factors

Stroke is a leading cause of disability in adults and the fifth leading cause of death, with close to 800,000 strokes occurring each year in the U.S. With an aging population, it is estimated that stroke will be the leading cause of death worldwide in the next few decades.
Who is most at risk for a stroke?
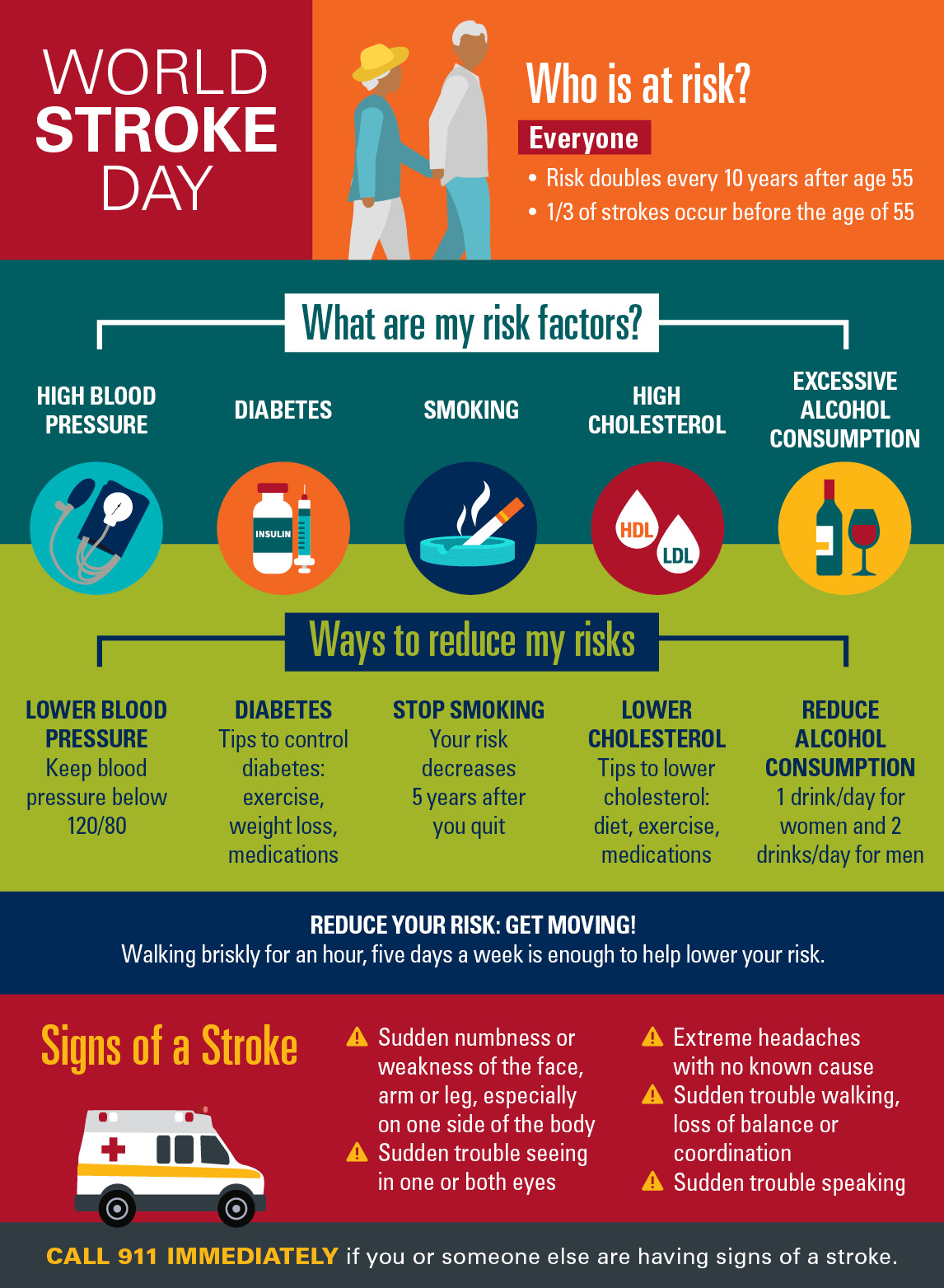
As you age, the risk of stroke increases significantly, doubling every 10 years after age 55. A common misperception, however, is that stroke happens only to older people. The truth is, while stroke is more common after the age of 55, no one is spared.
One-third of strokes occur before age 55 and can happen at any age. Women are just as susceptible as men, but on average, it usually hits women about 10 years later than men. Unfortunately, this age difference also puts women at greater risk of dying from stroke overall.
Today, we have more knowledge and effective ways to prevent stroke by controlling risk factors and using medications and interventions to prevent first and second-time strokes.
Everyone should be screened or evaluated for the risk of stroke after age 55. An initial screening involves a patient history and physical exam to gather information about risk factors and how to reduce them.
If you want to know if you are at risk for stroke, ask yourself the following questions:
Have I ever had a stroke or a transient ischemic attack, also known as a TIA?
Anyone who has had a stroke or TIA is at highest risk for a stroke. A TIA results from a sudden but temporary interruption of the blood supply to a brain region resulting in symptoms that last several minutes and, rarely, several hours. It is not associated with permanent brain damage; therefore, it is an ideal warning for a stroke.
Individuals who have experienced a TIA have a 10% chance of developing a stroke within the next 90 days, though many will have a stroke in the following 48 hours. If a person has experienced a TIA, they should work with their doctor to be evaluated and treated to prevent a stroke.
Do I have an irregular heartbeat?
Check with your doctor to see if you have atrial fibrillation or AFib, a specific type of irregular heartbeat. You can take your pulse to see if it is regular or irregular. If it is irregular, you should talk to your doctor. Many smartwatches or technologies reliably detect an irregular pulse, but atrial fibrillation needs to be thoroughly evaluated and identified as treatments are effective but can be associated with bleeding risks.
If you have AFib, your risk of stroke will increase significantly by an average of 5% per year. However, an appropriate treatment with oral anticoagulants, like warfarin or other newer medications, can reduce the risk by up to 80% despite potential risks.
Are the major blood vessels in my neck narrowed?
If so, intensive treatment with medications and specific intervention or surgery in selected persons can dramatically reduce your risk for stroke, depending on if they are causing symptoms or not, in addition to other factors.
Do I have abnormally elevated cholesterol or other fats in my blood?
Elevated cholesterol is more strongly associated with heart disease than stroke, but it does contribute to increasing the risk of stroke. Medications can significantly lower cholesterol and lower the risk of future stroke by about 16% in those with a prior stroke.
Am I a smoker?
Smoking tobacco, in all its forms, increases the risk of heart disease and stroke. It can also contribute to narrowing of the arteries in the neck and inside the skull. The good news is there are indications that five years after stopping smoking, the risk decreases significantly.
Do I have diabetes? Am I predisposed to diabetes?
Controlling diabetes with medications, diet, weight loss and exercise can significantly reduce your risk of stroke and heart disease. Even if you do not have full-blown diabetes, being predisposed to diabetes (insulin resistance) increases the risk of stroke. Treating patients with stroke and insulin resistance with diabetes medication significantly lowers the risk of stroke. If you are at risk for diabetes, you should know that diabetes can be prevented.
Is my blood pressure high? Am I predisposed to hypertension?
Hypertension is responsible for more than half of all strokes. Even if you do not have hypertension but other family members do, this may raise your risk of developing it. If you do not check your blood pressure, you will not know if you have hypertension since it does not cause specific recognizable symptoms. Check your blood pressure frequently and discuss your risk with your doctor. Ideal blood pressure is below 120/85 and should be the target of treatment for hypertension. Losing weight, lowering salt in your diet, adopting a diet rich in vegetables and fruits and exercising will prevent or lower hypertension.
Do I have heart disease?
Maintaining a well-functioning, healthy heart through regular physical activity and a healthy lifestyle and preventing a heart attack is an effective strategy for lowering the risk of stroke.
Do I drink alcohol excessively?
Excessive alcohol drinking, particularly binge drinking over weekends or other periods, can significantly increase the risk of hemorrhagic and ischemic stroke. Moderate alcohol intake (one drink/day for women and two drinks per day for men) is reasonable but may not reduce the risk of stroke and heart disease.
Am I too physically inactive?
Lack of regular exercise increases the risk of stroke and heart disease. It also increases the risk of obesity, hypertension, diabetes and high cholesterol. Moderate exercising, like brisk walking for an hour, or at least a half hour, five days a week, is enough to lower your risk. You do not need to run marathons to decrease the risk of stroke.
What are the major warning signs and symptoms of a stroke?
If you are at risk for stroke, you need to know the symptoms, recognize them, and plan with your family and friends how your stroke should be handled.
Stroke symptoms include:
- Sudden numbness or weakness of the face, arm or leg, especially on one side of the body
- Sudden trouble speaking or understanding speech
- Sudden trouble seeing in one or both eyes
- Sudden trouble walking, loss of balance or coordination
- Extremely severe headaches with no other known cause
Not all these warning signs occur in every stroke. If at least one does, don’t wait. Get help immediately.
What do I do if I recognize that I or someone else has stroke symptoms?
CALL 911 IMMEDIATELY!!!
Why? Because there are extremely effective treatments once a stroke happens, but they must be given within a few hours after the stroke occurs, preferably in a recognized, specialized, certified stroke center. The earlier the treatments are given the better the outcomes.
Treatments include:
- Intravenous tPA, or a clot buster, must be given within four and a half hours, and sometimes longer in some circumstances. But the earlier it is given, the more effective it is. Not all patients are candidates for this treatment, and the benefits must be higher than the bleeding risks it may cause.
- Another super-specialized treatment consists of placing a catheter in the groin and threading it into the blood vessel in the brain that is blocked, opening a “stent” (a cylindrical metal mesh), and pulling the clot outside the body to restore blood flow to the brain. The procedure is called mechanical thrombectomy, and it must be done within 24 hours. Not all patients are candidates for this procedure.







