What is steatotic (fatty) liver disease, and how does it affect the body?
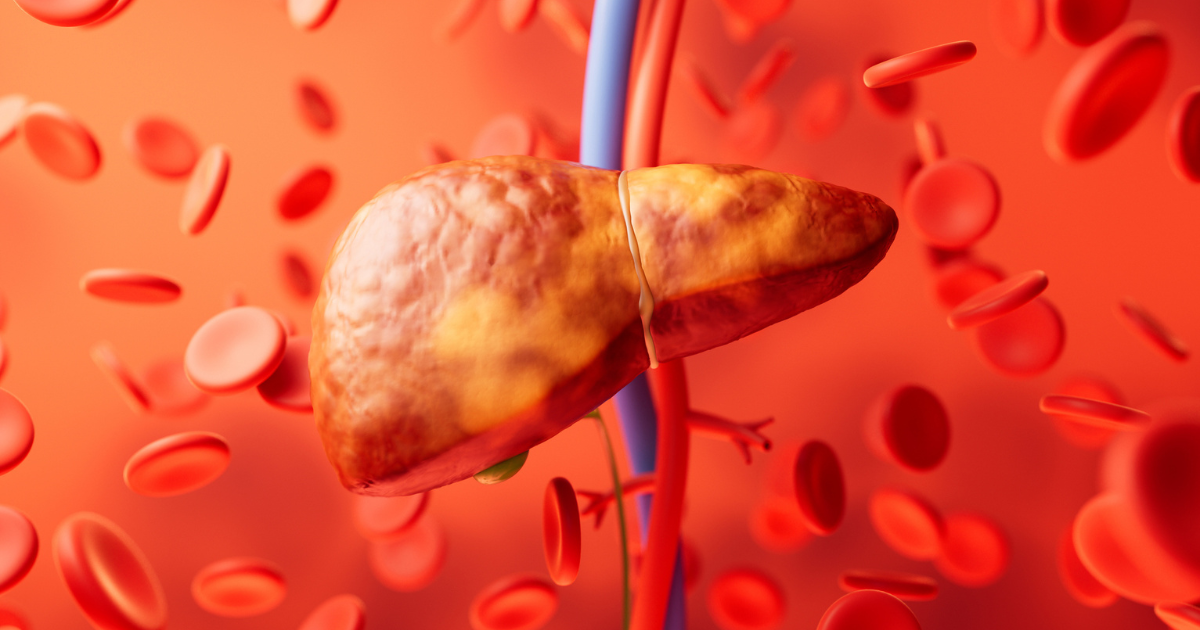
The condition, formerly called fatty liver disease, is now called steatotic liver disease as an umbrella term. Steatosis is a medical term that health care providers use to describe a fat buildup in an organ – in this case, the liver. The most common reason for this is MASLD (which used to be known as nonalcoholic fatty liver disease), which stands for metabolic dysfunction associated steatotic liver disease.
“This new umbrella term helps us get away from stigmatizing a serious condition,” says transplant hepatologist Faruq Pradhan, MBBCh. “We want to be accurate in our diagnosis for patients and avoid the use of stigmatizing terminology.”
Risk factors of steatotic liver disease/MASLD
Risk factors for MASLD that increase your likelihood of developing the condition include:
- Diabetes
- High blood pressure
- High total cholesterol or low numbers of good cholesterol
- High triglycerides
- Excess weight
- Smoking
“Generally, these cardiometabolic risk factors – the same risk factors that increase the likelihood of a heart attack – can also negatively affect your liver,” says Dr. Pradhan. “Also, if you’re drinking and have any of these risk factors, alcohol consumption can accelerate your chances of developing scarring, which can turn into cirrhosis (significant liver scarring that can affect liver function) over time.”
“This can be a silent process,” says Dr. Pradhan. “You can have fat in your liver and normal liver enzymes on your blood work, so the two don’t necessarily correlate.”
Symptoms of MASLD
Unfortunately, there aren’t many noticeable clinical symptoms of steatotic liver disease. Because of the lack of symptoms, this disease can be challenging to detect and diagnose early. “The disease progresses from you having fat in your liver and minimal or no inflammation to actually developing scarring,” says Dr. Pradhan.
Often, providers will diagnose steatotic liver disease incidentally when patients get an ultrasound or CT of their abdomen due to abdominal pain. The colon, stomach, kidneys and small bowel are all near the liver and are much more likely to cause pain than the liver. “So, there are a lot of other organs that can cause pain and erroneously make people think it’s their liver,” says Dr. Pradhan.
Even scarring doesn’t necessarily produce symptoms until it progresses to cirrhosis. “Liver scarring can be rather silent because it’s a tolerant organ,” says Dr. Pradhan. “Your liver can still function even if there’s scarring until it reaches a tipping point. This difficulty in recognizing steatotic liver disease early is why it’s quickly becoming one of the leading causes of liver transplants in the U.S.”
Preventing MASLD
“The number one prevention technique, with or without medication, is weight loss,” says Dr. Pradhan. “Losing weight and controlling other risk factors (stopping smoking, controlling diabetes, etc.) is invaluable.” Dr. Pradhan recommends patients aim to lose 7% to 10% of their total body weight. Losing this amount of weight can pull fat out of the liver, reduce inflammation and even potentially improve mild scarring of the liver.
“So, eating better and losing weight tends to be the best solution,” says Dr. Pradhan. “But I would never recommend someone buying over-the-counter weight loss supplements, as they can cause a whole other host of issues.”
Additionally, one relatively new drug – resmetirom (Rezdiffra™) – has been shown to help patients who already have moderate to significant liver scarring. This drug can help reduce fat in the liver, thereby decreasing inflammation.
“Currently, it’s the only drug on the market specifically indicated by the FDA to assist with steatotic liver disease,” says Dr. Pradhan. “But if you have no scarring – or your disease has progressed to cirrhosis, the drug isn’t approved for that population yet.”
Diagnosing and treating MASLD
“Typically, we diagnose someone with steatotic liver disease by finding elevated liver enzymes in their blood work or when they get imaging like a CT scan for another reason, and we accidentally discover the condition,” says Dr. Pradhan.
One of the tools Nebraska Medicine providers have to help diagnose steatotic liver disease is a FibroScan®. “This noninvasive tool uses a probe placed on your skin between your ribs and allows us to see how much scarring and fat there is in your liver,” says Dr. Pradhan.
Still, because of the potential lack of symptoms of steatotic liver disease, prevention and early recognition are vital to defeating the disease. “Recognizing any signs of the condition and working on weight loss or reversing any other pre-existing metabolic conditions or diseases is essential as it will also help prevent steatotic liver disease,” says Dr. Pradhan. “For example, adopting a Mediterranean diet is generally preferred. I recommend it to patients as it effectively lowers high blood pressure.”
Reducing the need for liver transplants
According to Dr. Pradhan, over 10,000 liver transplants occurred nationwide in 2023. “But there certainly aren’t enough livers to go around if 30% of the population has MASLD,” says Dr. Pradhan. “So, we have to keep hammering prevention points, especially because other causes of liver disease have fallen, and steatotic liver disease is now one of the leading causes of transplants.”
Additionally, liver transplants are further complicated for those with steatotic liver disease because the transplant drugs patients take to protect their new liver can also increase blood pressure and sugar. Consequently, these drugs increase your risk of developing fat in the liver after a transplant – even if it wasn’t the reason why you needed a transplant in the first place.
Because of these issues – and the lack of pain receptors in the liver, resulting in a lack of symptoms, preventing steatotic liver disease remains paramount. “Steatotic liver disease being asymptomatic often leads to patients shocked to discover they already have cirrhosis in some cases,” says Dr. Pradhan. “So, the best thing is prevention.”






