Second chances: Telestroke Program offers critical expertise to small towns
Roger Edwards had always been a kidder. So when his wife, Jackie, found him on the floor next to the bed, she thought it was another prank. But she quickly realized that Roger wasn’t moving. Nor was he responding. Jackie picked up the phone and called 911.
An ambulance arrived immediately and took him to the nearest hospital – UnityPoint Health – St. Luke’s in Sioux City, Iowa. “I tried to stay calm and not panic,” recalls Jackie. “But when the hospital ER staff asked me if I wanted to send him to Omaha or let him go, I knew it was serious.”
To schedule an appointment with a neurologist on our stroke team, call 800.922.0000.
Roger had suffered the most severe form of stroke – a basilar artery occlusion stroke. With this type of stroke, the blood clot blocks the largest vessel that supplies the brainstem. It carries a high risk of mortality, or severe disability, if you survive.

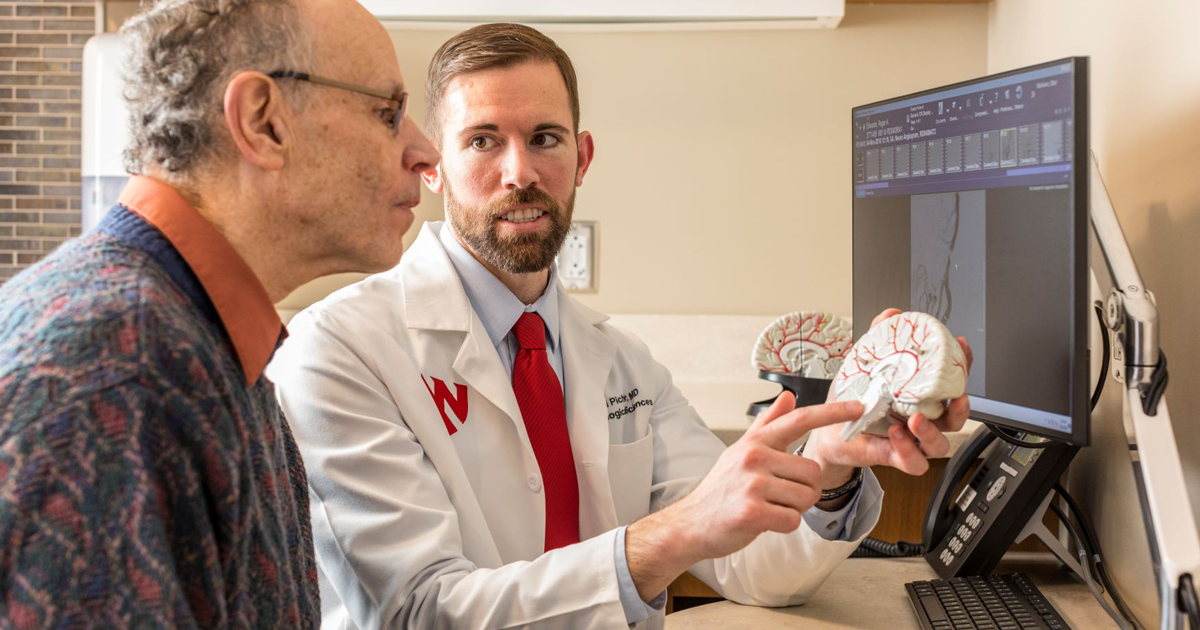
“It’s one of the types of stroke we fear the most,” says Michael Pichler, MD, Nebraska Medicine neurologist. Dr. Pichler was the neurologist on call that day at the Nebraska Medical Center. St. Luke’s is one of eight Nebraska hospitals that are part of the Nebraska Medicine Telestroke Program. As members of this program, these hospitals have immediate access to the Nebraska Medicine stroke team for quick assessment of stroke patients who come to their hospital. After the Nebraska Medicine stroke team was contacted, Dr. Pichler immediately remoted in via video monitors. Within a few minutes, he had assessed Roger and recommended administration of tPA (a blood thinning drug that helps dissolve the clot) to buy him time to make the air transport to Nebraska Medical Center for emergency stroke surgery.
“As soon as I saw the results of his CT angiogram, I could see that a large segment of his basilar artery was completely blocked, and as a result, would be a candidate for thrombectomy,” says Dr. Pichler. “But he needed to get here fast.”
Mechanical thrombectomy is an advanced vessel-opening procedure performed by trained endovascular neurosurgeons. Using high tech imaging equipment, the procedure involves threading a catheter through the femoral artery to the site of the clot. The stent is used to remove the clot so blood flow can be restored to the brain.
When Roger arrived at Nebraska Medical Center, the stroke team was waiting. Daniel Surdell, MD, a Nebraska Medicine cerebrovascular and endovascular surgeon, performed the mechanical thrombectomy procedure. “Once we received word that Roger was being transferred here, our stroke team was deployed and ready,” says Dr. Surdell. “Time is critical when it comes to stroke. Our goal is to treat the patient quickly and appropriately to reduce the amount of damage caused by the stroke as much as possible.”
“I was amazed at how quickly they got things going,” says Jackie. “They immediately took him into surgery and shortly after the procedure, he was moving around and answering questions. The next day while he was in the intensive care unit, he even gave one of the nurses a high five!”
“The first memory I have is walking down the hallway, carrying my walker instead of using it,” says Roger. “Even the doctors said they were amazed that I had made it and was doing so well.”
Performing the thrombectomy procedure probably saved his life, or at the very least, has allowed him to enjoy quality of life,” says Dr. Pichler. “This type of stroke can leave a patient completely paralyzed in all extremities and unable to communicate.”
Drs. Surdell and Pichler are backed by a team of health care providers whom have a wealth of experience and stroke expertise. The team also includes two additional vascular neurologists, a neurohospitalist, stroke nurse and neurointensivist. They are part of the only certified Comprehensive Stroke Center in the region, the highest level of stroke certification available. It is the only stroke team in the area equipped to handle the most complex stroke cases and provide specialized around-the-clock treatment 24 hours a day, seven days a week.
“We have seen a lot of success stories due to the telestroke program,” says Dr. Pichler. “This program allows small hospitals that do not have neurology or stroke neurology on staff to have access to 24/7 stroke expertise through Nebraska Medicine. It allows us to quickly assess and appropriately diagnose patients and provide potentially life-saving interventions.”
Because of the quick diagnosis and treatment performed by the Nebraska Medicine stroke team, Roger survived his stroke and has recovered remarkably well. Aside from driving, due to a blind spot in each eye caused by the stroke, Roger says he can do just about everything he could before the stroke.
“Whatever they are doing, they need to keep doing it,” says Roger. “They did an excellent job and as a result, they gave me a second chance.”




