Trial aims to improve Parkinson's patients' sleep

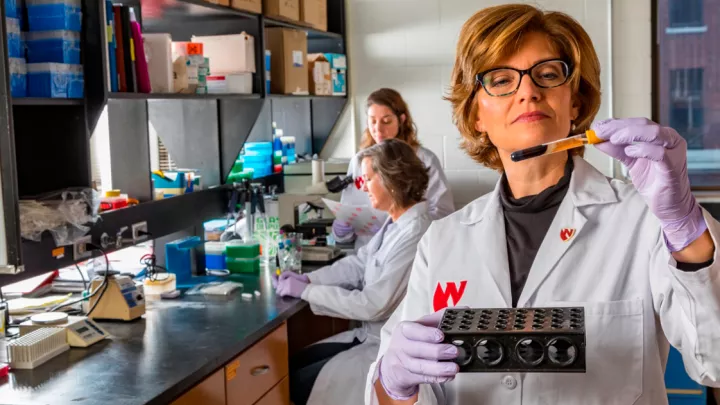
Early in her career, neurosurgeon Aviva Abosch, MD, PhD, began receiving surprising feedback from Parkinson’s patients on whom she had operated.
“They would come back to my clinic and say, ‘Thanks for your help with my tremor, but I really want to thank you for helping my sleep. I'm sleeping better than I have in the past decade,’” Dr. Abosch says.
Her patients’ surgeries were only meant to improve the motor symptoms of Parkinson’s disease, a disorder of the central nervous system that can cause uncontrollable movements, including tremors and rigidity. But somehow, many were sleeping better.
“I thought that was weird, so I started educating myself about sleep and Parkinson’s disease,” Dr. Abosch says. “It turns out that as many as 98% of patients with Parkinson’s disease have wildly disrupted sleep.”

Not only can patients not stay asleep, repeatedly waking all night, but they have diminished rapid eye movement, or REM, sleep and non-REM stage 3 sleep, the two components of healthy sleep that help us feel rested when we awaken in the morning. These are also the stages of sleep during which our bodies repair damage to our central nervous system.
“It’s a double hit,” Dr. Abosch says. “You have an ongoing neurogenetic disorder, and, in addition to that, your sleep declines drastically.”
After hearing the same thing from many patients, Dr. Abosch began to wonder if there was a measurable improvement in their sleep following deep brain stimulation, or DBS, surgery for their Parkinson’s disease. And, if so, was there a way to leverage that improvement into even better sleep?
The trial
Abosch enlisted a sleep expert from Standford University, Clete Kushida, MD, PhD, to help her team study how the brain works during sleep. In the first part of their trial, Dr. Abosch’s team identified brain activity patterns tied to specific stages of sleep, with these patterns serving to identify the specific sleep stages. Now, they are testing how stimulating a specific part of the brain with a pacemaker-like device can best help improve Parkinson’s patients’ sleep in addition to their movement symptoms.
The implications of their findings could be huge for Parkinson’s patients and their caregivers, who are often significantly impacted by sleep problems.
“Taken together, the non-motor symptoms can be much more burdensome to patients than the motor symptoms,” Dr. Abosch says. “Of the non-motor symptoms, sleep is the biggest one. Because of the repeated waking and movement during REM sleep – when your brain is supposed to prevent movement so that we cannot act out our dreams – patients and their spouses stop sleeping together, which is a huge burden on them both.”
The trial is for Parkinson’s patients with a deep brain stimulation device already implanted for their motor symptoms. As part of the trial, they receive different types of targeted stimulation, which the team hopes will help patients have:
- More consolidated sleep
- Fewer nighttime awakenings
- More REM and slow-wave, non-REM stage 3 sleep
- Less daytime sleepiness
- Better overall sleep quality
Additionally, the team’s findings could help other patients with sleep problems, which are common in other neurodegenerative diseases, such as dementia, and neuropsychiatric disorders, such as schizophrenia.
The study is sponsored by the National Institute of Neurological Disorders and Stroke and supported by the National Institute of Health’s Brain Research Through Advancing Innovative Neurotechnologies (BRAIN) Initiative, whose goal is to revolutionize understanding of the human brain.
For more information, email Dulce Maroni Veiga, PhD, at dmaroni@unmc.edu.
IRB number: 577-21-FB
Cinicaltrials.gov NCT04620551