Epilepsy and deep brain stimulation
Epilepsy is a neurological disorder that causes recurrent seizures and can significantly impact an individual's quality of life. Anticonvulsant medications don’t control seizures well for about one-third of patients with epilepsy. For some of these patients, deep brain stimulation, or DBS, is a promising therapy.
DBS involves implanting electrodes, or leads, in specific regions of the brain, to deliver electrical impulses that regulate abnormal brain activity known as seizures. Originally developed for treating movement disorders such as Parkinson's disease, DBS has proven successful in reducing seizures in patients with refractory epilepsy, or epilepsy that is resistant to medication.
“The epilepsy population in whom we implant deep brain stimulators have failed multiple drug regimens for the treatment of their epilepsy, and the anticonvulsant medications have been pushed to toxicity in most cases,” says neurosurgeon Aviva Abosch, MD, PhD. “These patients are still having seizures, which are life-threatening.”
DBS is typically reserved for patients who have multifocal epilepsy, meaning there is not one single location that is producing seizures. Instead, seizures start from several different areas of the brain.
How DBS works
Patients undergoing DBS treatment can expect the following from surgery through the DBS device programming:
-
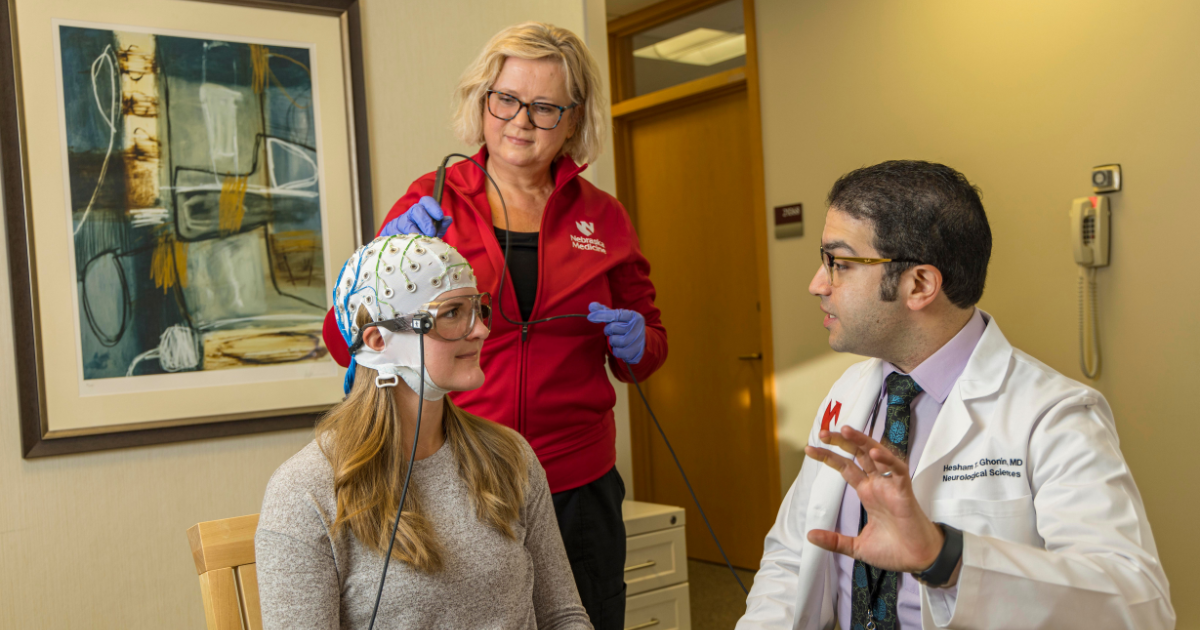
Before surgery, scalp EEG, neuropsychological testing, and various brain imaging studies are completed to help the Multidisciplinary Epilepsy Team determine whether or not DBS is the appropriate treatment for a patient’s epilepsy.
-
At the beginning of the procedure, the patient is placed under general anesthesia.
-
Incisions are made in the scalp small holes are drilled through the skull, and the leads are implanted into the brain.
-
Leads are implanted in the brain’s right and left hemispheres, guided by the previously obtained images.
-
The leads are connected to extension cables that run underneath the skin of the scalp, neck and chest and are connected to a battery-powered neurostimulator underneath the skin in the chest.
-
When the patient has healed from surgery, a programming clinician adjusts the settings of the neurostimulator.
-
Once programmed, the device delivers electrical stimulation to the brain, modulating abnormal neuronal activity to treat the patient’s seizures.
Nebraska Medicine neurosurgery teams perform the DBS procedure on carefully selected adults with drug-resistant epilepsy who do not have medical problems that would make surgery risky.
“The surgery to implant the stimulators is not nearly as invasive as other things we do in neurosurgery. If a patient is determined to be a candidate for this therapy, can tolerate being under a general anesthetic and is willing to undergo the DBS procedure, then we proceed with surgery,” Dr. Abosch says.
Effectiveness of DBS
While DBS has been shown to reduce seizures by nearly 50%, all patients respond differently; for some, it may be as high as 70%. In addition, DBS can improve a patient's quality of life by enabling the epilepsy neurologist to reduce seizure medications, reducing medication side effects and allowing for better seizure control.
“We think of DBS as a palliative procedure, meaning it is not curative, but is aimed at alleviating seizure burden and perhaps reducing medication use and some of the side effects that come with medication,” says epilepsy neurologist Olga Taraschenko, MD, PhD.
While some patients experience immediate improvement following DBS placement, most experience incremental improvement over many months, which peaks around two years after surgery.
“It’s a long process,” Dr. Taraschenko says. “We tell patients to wait three to six months before worrying whether the neurostimulation is working or not.”
While DBS offers hope for patients with refractory epilepsy, it is not without risks. Potential complications include:
-
Infection
-
Bleeding
-
Worsening of depression for some patients who were already experiencing depression before the device was implanted
-
Memory impairment
-
Tingling on the scalp
Despite these challenges, DBS represents a significant advancement in treating refractory epilepsy. While Nebraska Medicine neurosurgeons have performed DBS surgery for decades for other conditions, such as Parkinson’s, the surgery was only approved by the US Food and Drug Administration for the treatment of epilepsy in 2018. This summer, the Nebraska Medicine Comprehensive Epilepsy Program –including a team of neurologists, neuropsychologists, neuroradiologists, and neurosurgeons – brought its first epilepsy patient through the evaluation process, DBS surgery, and device programming.
“Previously, we have had to send patients out of state for this surgery, so it’s exciting that we can now provide it here,” Dr. Taraschenko concludes.