A veteran's journey through lung cancer

Jake White, an Army veteran who recently battled lung cancer, is living proof of the vital role that cancer screening and early detection plays in saving lives. White’s 40-year smoking history, coupled with a family history of cancer, prompted his Veterans Administration health care provider to recommend regular CT scans of his lungs. This proactive approach proved instrumental in diagnosing his illness at a treatable stage.
“In the CT scan before finding the cancer, there was just a cyst,” says White, 58. “Three months later, in September 2022, they found the cancer. Having those scans allowed them to catch it and attack it early, so the cancer couldn’t spread further.”
White and his wife, Renee, turned to Nebraska Medicine doctors to treat the advanced nonsmall cell cancer in his left lung. In December 2022, White underwent surgery to remove the tumor. However, thoracic surgeon David Berkheim, MD, discovered the cancer had spread to the lining of the lung and halted the surgery.
“Though, this meant he was now stage IV, given his young age and limited spread, we decided to be fairly aggressive and planned chemotherapy and immunotherapy followed by resection,” Dr. Berkheim says.
White's treatment plan involved six rounds of chemoimmunotherapy, a combination of chemotherapy and immunotherapy, which shrank the tumor. It was removed in June 2023, and White has remained cancer free. He undergoes scans every three months to monitor his status.
Throughout White’s journey, he found solace and support in his wife, two sons, friends, church community and Christian faith.
“My wife and kids were extremely supportive, and my friends took turns visiting me during chemo sessions,” White says. “If we needed anything, church members would jump in and help. They did a meal train during the chemo, and everybody was very supportive.”
Coping with trauma
As a combat veteran, White carries the weight of posttraumatic stress disorder stemming from a deployment in Northern Iraq, where he sustained serious injuries. Smoking cigarettes served as a coping mechanism.
In 2018, White decided to quit smoking and turned to art to fill the void left by the habit. He found a therapeutic release using a tablet to create digital charcoal and graphite drawings, primarily religious themes. His illustrations became a way to express his feelings, and he eventually led a team of artists from his church in an art project focused on the Tenebrae service that proceeds Lent.
“I grew up drawing, but then I just kind of stopped,” he says. “In 2018, I was like, ‘I need to do something other than smoking,’ so I started drawing again. It surprised my wife and my church community because I was always known as the tough guy who doesn’t have a lot of emotions, so it was a funny, interesting surprise to them.”
On White’s website, he publishes his images and sells prints of his work. While undergoing chemotherapy, White felt fatigued and was unable to draw. As he recovers from treatment and surgery, he hopes to return to drawing, as well as regain the strength and energy to practice fencing with his 13-year-old son, Spencer, and play baseball with his 10-year-old son, Henry.
The importance of screening
White encourages fellow veterans to seek early detection through cancer screenings, particularly if they smoke. According to the American Lung Association, 21.6% of military veterans smoke, compared to 14% of nonveteran U.S. adults.
“A lot of veterans, especially combat veterans, feel like, ‘I’m stronger than that. I don’t need to have a test,’” White says. “I understand, and I felt that way, too. But get the first scan done and go from there.”
Medical oncologist Omar Abughanimeh, MBBS, who treated White, agrees.
“Around half of the lung cancer cases we see in our clinics are Stage 4, which is not a curable stage in most cases,” he says. “Screening with low-dose CT scan allows us to detect cancer in early stages when a curable treatment can be offered.”
Just as a mammogram, blood pressure check or colonoscopy screening can be lifesaving, the same holds for annual lung cancer screenings for those who meet the criteria.
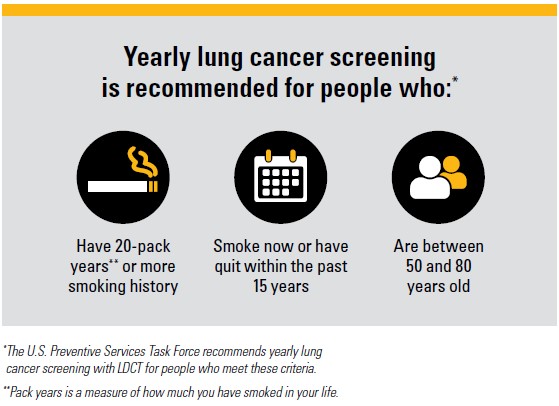
Nebraska Medicine’s Comprehensive Lung Cancer Screening Program is a multidisciplinary collaborative to improve lung cancer screening. To serve our patients in the program, we use a team of radiologists, pulmonologists, thoracic surgeons, medical oncologists, smoking cessation experts, researchers, primary care providers, and nurses to develop a best-practice, patient-centered plan.
There is a lot of room to improve the rates for lung cancer screening and Nebraska Medicine’s program wants to make it as easy as possible for patients at risk to get screened.







