Transcranial magnetic stimulation: Can it actually help with depression?

Transcranial magnetic stimulation, or TMS, is a breakthrough treatment for those with chronic, medication-resistant depression. FDA-approved treatments began in 2008 and have continued for 14 years with encouraging results. Exciting research is ongoing in hopes of possible future uses beyond depression, including anxiety, OCD, addiction, PTSD, and other mental health conditions.
Nebraska Medicine is preparing to offer TMS treatment to patients before the end of 2022 and is excited about the difference it can make for those who live with depression.
How TMS works
TMS stimulates the brain in targeted areas to decrease or eliminate depression symptoms. The treatment uses a series of short magnetic electrical pulses (also referred to as rTMS) to stimulate nerve cells in specific parts of the brain known to be associated with major depression.
The current comes from a weak magnetic field created by a cooled electromagnetic coil. The coil delivers a repetitive, oscillating magnetic field through the scalp. Because TMS produces a weak magnetic field, it generates a small electric field in the brain in specific areas, reducing side effects.
Who is a good candidate for TMS treatment?
You are eligible for TMS if you've had two medication trials for depression with minimal or no symptom improvement.
You will be screened for certain conditions to confirm eligibility and reduce potential complications. To be eligible, you must not have a history of:
- Bipolar disorder or other comorbid conditions
- Metal in the head above the ears
- Anything that puts you at higher risk of seizure, including epilepsy or other seizure disorder
Reducing depression symptoms: How effective is TMS?
The response rate is close to 60% for patients who have not responded to at least two medications. This is an impressive number, giving many suffering from medication-resistant depression hope of relief.
How to get TMS treatments at Nebraska Medical Center
Nebraska Medicine is in the process of developing a central hub for referrals and intervention. Currently, expect a two-step process to get started:
- Evaluation by your primary care physician or your psychiatrist, who will refer you for TMS treatment if you are eligible.
- Evaluation by a TMS specialist, who will schedule your treatments if eligible, walk you through the process and answer your questions. They will take measurements to find the least amount of pulse needed and locate the part of the brain to be treated at the lowest energy level.
What to expect when TMS treatment begins
You will begin your first treatment session the day after meeting with your TMS specialist.
- Expect about 35 to 40 minutes for the initial treatment
- You will be asked to wear ear protection and a cloth cap over which a magnetic coil will be placed.
- Plan to stay still during treatment. You can rest, listen to music or use an electronic device if you wish
- At any point, if you feel uncomfortable, let the technician know. They will be with you throughout the entire treatment
- You may experience a knocking sound or light tapping sensation during treatment. You may experience a mild headache that usually dissipates after 24 hours
- You will repeat your sessions five days a week for six weeks. Typically this means a total of 30 sessions or so, depending on how you respond. In the last week or so, your treatments will start to taper off
- You will stay on your medication during and after treatment
- Once treatment is complete, you will follow up with the doctor who referred you
Pros and cons of TMS therapy
Every person responds to TMS treatment differently.
Pros
- You'll see the technician every day, and your symptoms will be monitored regularly by a psychiatrist so changes in your TMS treatment can be made quickly.
- TMS uses a low-dose current, so side effects are minimal to none
- Your memory will not be impaired
- Treatment is safe, noninvasive and well tolerated
- You can return to everyday life immediately after treatment and do not need anyone to drive you to or from the clinic.
- You are not adding additional medications
- Time commitment is limited to the course of treatment
Cons
- Concentrated time commitment
- Some experience a temporary, mild headache or facial twitching during sessions
- Tapping or knocking sensation during treatment
Can TMS cure depression?
"Depression is a chronic condition with waves of remission and relapse," says Varun Sharma, MBBS, Nebraska Medicine psychiatrist. "It's not like a broken bone that is fixed or cured, but rather a chronic illness. The goal is remission to reduce symptoms and improve quality of life using the treatment with the least side effects. We want to lengthen the time we keep depression symptoms at bay."
If you've had a good response with TMS before, there's a good chance you would respond again if future treatments are needed for a reoccurrence of depression symptoms.
When TMS doesn't work
If you've gone through TMS and feel it didn't work for you, don't lose hope, you have options. "We need to ask ourselves, is it that TMS wasn't helpful and your depression isn't getting better, or is it not the right treatment for your particular situation," says Dr. Sharma. "Everybody is different. If TMS isn't helpful, we offer a complete spectrum of treatment options for treatment resistant depression to help with your depression and find the right treatment."
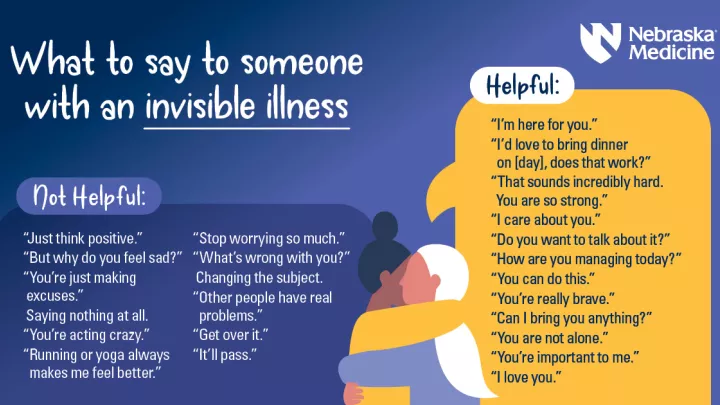
If someone you love struggles with depression, they need your validation and empathy. You can help by knowing how to respond in a helpful, supportive way.
Nebraska Medicine experts provide a wide array of mental health treatments and services, including connecting you to behavioral health resources for free. In 2021, Nebraska Medicine opened adult Psychiatric Emergency Services to provide immediate care by licensed mental health providers in a safe, private setting.
To make an appointment with a mental health specialist, call 800.922.0000.