Headaches: Why they happen and when they can be serious

Headaches can severely affect your quality of life and ability to function. They can be caused by a neurological disorder of the brain or other underlying diseases, which if not treated, could be life-threatening. Read on to learn how to identify different types of headaches and when to seek treatment.
Types of headaches and their causes
When classifying headaches, it is most important to determine whether the headache is primary or secondary. A primary headache, such as a migraine, is a complex neurological disorder where the brain is more excitable than individuals who do not have migraine.
Examples of primary headache disorders include:
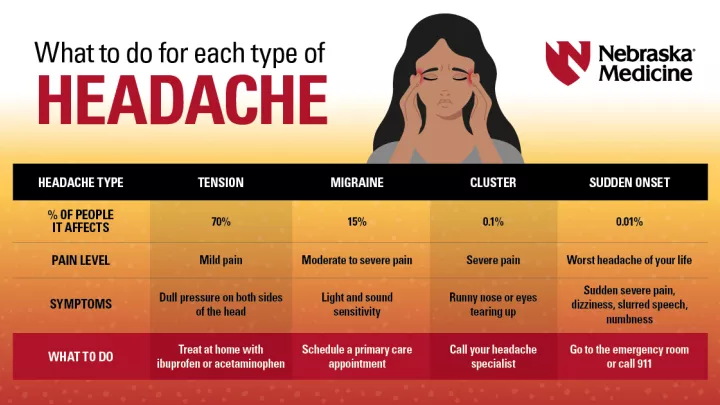
• Tension headaches – Associated with mild or moderate intensity of tightening or pressing quality on both sides of the head
• Migraine headaches – Can present as moderate or severe pulsating pain on the side of the head, with associated sensitivity to light and sound, nausea, or vomiting
• Cluster headaches – Symptoms include severe pain around the eye or temple with runny nose, tearing, swollen eyelid, facial sweating, decreased pupil or droopy eyelid that occur in clusters on the same side of the head
Primary headaches can have certain triggers or exacerbating factors, such as:
• Mood disorders
• Disruption in sleep or lack of sleep
• Skipping meals
• Foods that contain nitrates, MSG, artificial coloring, artificial sweeteners
• Poor posture
• Stress
“Women are three times more likely than men to experience migraine,” says Nebraska Medicine neurologist Peter Soh, MD, MPH. “There is also a misconception that pain around the sinuses is due to a ‘sinus headache.’ While headaches due to sinus infections exist, they are usually due to migraine, which sensitizes the nerves that supply the sinuses.”
A secondary headache is a symptom of an underlying disease that can inflame the covering of the brain, disrupt the nerve endings of blood vessels in the head and neck, or damage the nerves supplying the face or back of the head. Any number of conditions may cause secondary headaches, including:
• Autoimmune diseases
• Abnormal vitamin levels
• Hormone changes, such as fluctuations in estrogen and progesterone during pregnancy
• Infections
• Pressure changes of the fluid that surrounds the brain and the spinal cord
• Torn blood vessels
Symptoms that may be indicative of a secondary headache disorder include:
• A suppressed immune system or systemic symptoms, such as fever, unintended weight loss or night sweats
• A sudden headache that peaks in intensity within minutes
• Changes in headache pattern, including frequency, duration and symptoms
• New onset or worsening seizures
• Neurological symptoms, such as visual disturbances, numbness or weakness on one side of the body, difficulty with speech or imbalance
• A headache triggered by coughing, exertion, sexual activity, sleep or positioning
• Increased pressure in or around the brain that causes swelling of the part of the optic nerve inside the eye, a condition known as papilledema
“Patients who have headaches and COVID-19 typically display other symptoms, such as fatigue, muscle aches, sore throat, or even loss of taste and smell,” says Dr. Soh. “However, if a patient does not have a history of headaches and presents with a new headache, with or without these symptoms, then a workup for secondary causes or even COVID-19 is reasonable.”
How to safely manage headaches at home
Keeping a daily headache journal to track the frequency of your headaches, timing, potential triggers, therapeutic efficacy of medications, and, if applicable, menstruation, is the most cost-effective method to help manage your headaches.
Strategies for migraine prevention include:
• Getting adequate sleep
• Eating a balanced diet and not skipping meals
• Managing stress
• Staying hydrated
• Cardioaerobic exercise
When to seek medical treatment for headaches
Neurologists are doctors specially trained in the diagnosis and management of headaches. Consider consulting with a neurologist if you experience headaches that:
• Have become more severe or frequent
• Interfere with work, school or social activities
• Lead to an urgent care or emergency room visit
• Require taking medication for four or more days per month to treat acute symptoms
“Managing headaches requires a multifactorial strategy,” says Dr. Soh. “By partnering with patients, we can make correct diagnoses, find optimal treatment plans, and in time, improve their quality of life and functionality.”
Experiencing reoccurring headaches or migraines? Call 800.922.0000 to schedule an appointment.